Abstract
Introduction: MDS comprise a heterogeneous group of hematological malignancies with 10,000-20,000 cases diagnosed in the US annually. Although erythropoiesis-stimulating agents are often used in lower-risk (LR) MDS, 3 agents are approved for the treatment of MDS in the US: HMAs (azacitidine and decitabine) and LEN. Given the limited response rates and ultimate treatment failure with these drugs, they are used in sequence. Despite being available for over a decade, there are little data on the impact of their sequencing on clinical outcomes. One small single-center study by Zeidan et al (2015) in 63 patients with non-del(5q) LR-MDS concluded that LEN is optimally positioned before azacitidine when the drugs are in sequence. The current study aimed to look at this question using a real-world MDS patient dataset not restricted to non-del(5q) LR-MDS patients who were treated with an HMA followed by LEN (HMA-LEN) or LEN followed by an HMA (LEN-HMA).
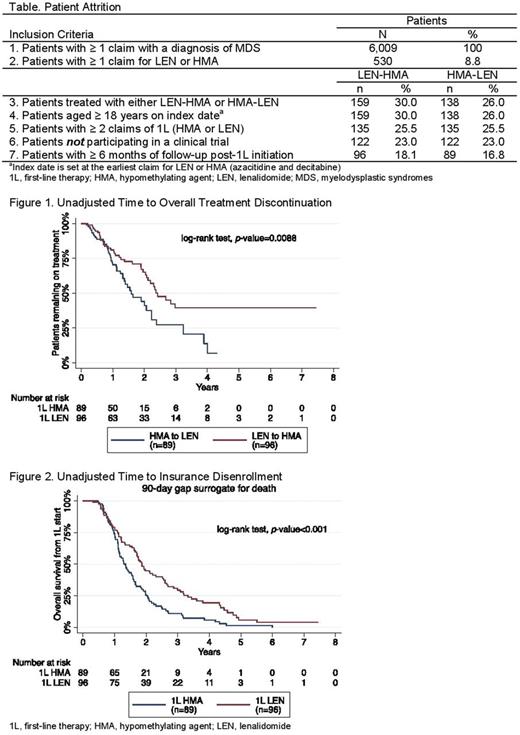
Methods: Adults with a diagnosis of MDS (ICD-9: 238.72-238.75 and ICD-10: D46) were identified from a large US payer claims database from Jan 1, 2008 to Dec 31, 2016. The index date was defined as the first claim for LEN or HMA as first-line therapy (1L). Patients had to have ≥ 2 claims of their 1L and ≥ 1 claim of second-line therapy (2L), with ≥ 6 months of follow-up data available from index date. Patients in a clinical trial were excluded. Transfusion dependence (TD) was defined as ≥ 2 claims for transfusion event during an 8-week period at any time prior to start of 1L (with ≥ 1 claim within the 8-week pre-index period) or within 90 days of start of 1L. Transfusion independence (TI) was defined as ≥ 8 weeks without a claim for a transfusion event. Overall treatment discontinuation was identified when there was a ≥ 90-day gap between last claim in last line of therapy and end of follow-up or study period. Date of insurance disenrollment was identified in patients with a ≥ 90-day gap from last observed claim for any healthcare resource to end of data availability. As date of death was not available, time from index date to date of insurance disenrollment served as a proxy for survival with the assumption that older patients with chronic conditions are unlikely to change insurance and have high healthcare burden. Time from index date to discontinuation and disenrollment were adjusted for potential confounders at start of 1L. The covariates used in Cox proportional hazard models included gender, age, payer, region, Charlson Comorbidity Index, cytopenias (anemia, thrombocytopenia, neutropenia), and the SEER-Medicare MDS Risk Score (SMMRS) category (a proxy measure for the International Prognostic Scoring System developed for SEER-Medicare MDS analyses).
Results: Out of 6,009 MDS patients, there were 89 HMA-LEN patients and 96 LEN-HMA patients (Table); 41 (46%) and 46 (48%) were TD at initiation of 1L, respectively. Median age was 74 years for both groups. The LEN-HMA patients had a lower rate of cytopenias at baseline (29.2% vs 12.5%; P= 0.005) but similar distribution of SMMRS categories (P= 0.161). Patients treated with LEN-HMA had a longer time to overall treatment discontinuation (29.0 vs 19.0 months; P= 0.009; Fig 1) and a lower adjusted risk of treatment discontinuation (hazard ratio [HR] 0.52; 95% CI 0.29-0.91; P= 0.023). Among patients with TD, rates of TI were directionally higher in the LEN-HMA cohort during 1L (37.0% vs 34.1%), 2L (41.3% vs 22.0%), and overall therapy (56.5% vs 46.3%; P= 0.343), but were not statistically significant. Alternatively, examining the mean number of transfusions 6 months prior to and after 1L initiation showed no difference before treatment (1.68 vs 1.99; P= 0.452), but while on therapy, the LEN-HMA cohort had a lower transfusion frequency (2.10 vs 3.98; P= 0.002). Looking at survival in relation to insurance disenrollment, median time to disenrollment was longer in LEN-HMA patients (1.87 vs 1.34 years; P < 0.001; Fig 2), and these patients had a lower adjusted risk of disenrollment (HR 0.64; 95% CI 0.44-0.92; P= 0.017).
Conclusions: Patients receiving LEN-HMA remained on treatment longer and had lower frequency of transfusions while on therapy. These patients also demonstrated additional clinical benefit through improvements in survival, as measured by the proxy of adjusted time to insurance disenrollment. Observational data from a nationally representative database directionally confirm the benefits of the LEN-HMA treatment sequence in MDS patients.
Zeidan: AbbVie, Otsuka, Pfizer, Gilead, Celgene, Ariad, Incyte: Consultancy, Honoraria; Takeda: Speakers Bureau; Otsuka: Consultancy. Klink: Cardinal Health and HealthCore (Anthem): Employment; Janssen, BMS, Celgene, EMD Serono, Ipsen, Kite, Merck, Novartis, Vertex, Amgen, Astellas, Heron, AbbVie, Array: Consultancy. Feinberg: Cardinal Health: Employment. McGuire: Celgene: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal